Infectious diseases are illnesses caused by harmful organisms (pathogens) that infiltrate your body. Some examples of these pathogens that cause infectious diseases are viruses, bacteria, fungi, parasites and prions. Let’s break them down:
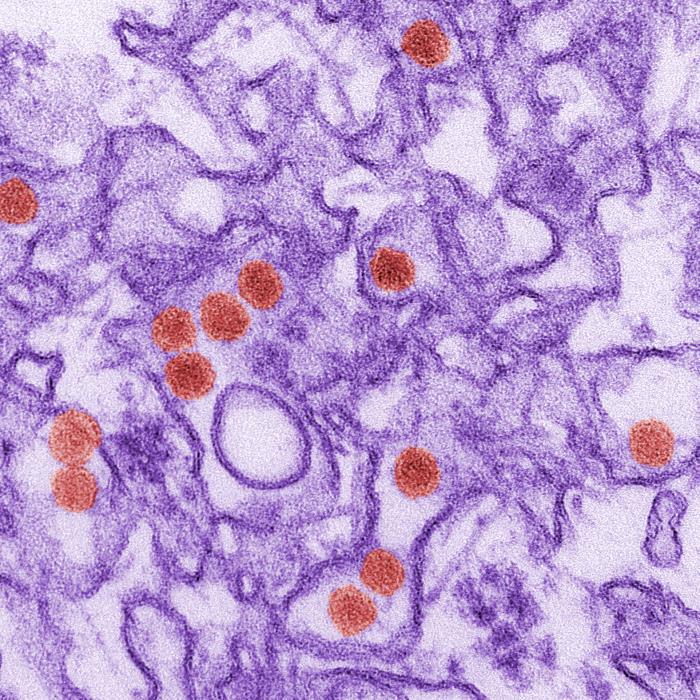
- Viral infections. Viruses are a piece of information (DNA or RNA) inside of a protective shell (capsid). Viruses are much smaller than your cells and have no way to reproduce on their own. They get inside your cells and use your cells’ machinery to make copies of themselves.
- Bacterial infections. Bacteria are single-celled organisms with their instructions written on a small piece of DNA. Bacteria are all around us, including inside of our body and on our skin. Many bacteria are harmless or even helpful, but certain bacteria release toxins that can make you sick.
- Fungal infections. Like bacteria, there are many different fungi. They live on and in your body. When your fungi get overgrown or when harmful fungi get into your body through your mouth, your nose or a cut in your skin, you can get sick.
- Parasitic infections. Parasites use the bodies of other organisms to live and reproduce. Parasites include worms (helminths) and some single-celled organisms (protozoa).
- Transmissible spongiform encephalopathies (TSEs/prion diseases). TSEs are caused by prions — faulty proteins that cause other proteins in your body, usually in your brain, to become faulty as well. Your body is unable to use these proteins or get rid of them, so they build up and make you sick. Prions are an extremely rare cause of infectious diseases.
Source: https://www.my.cleveland.org
Below are some common infectious diseases that you should become familiar with. We have also included some rare ones because it is always good to be aware of what’s lurking microscopically around us!
What’s Plaguing Us? Podcast
Be on the lookout for our podcast What’s Plaguing Us? featured on the UM Libraries’ Roundabout Oxford Podcast! Hosted by our University Health Services Director, Alex Langhart, What’s Plaguing Us covers public health topics focusing on infectious diseases throughout history and how humanity has been impacted. Segments will be posted to this page along with the link to the full Roundabout Oxford Podcast!
EPISODES
COMMON COLD
Sore throat and runny nose are usually the first signs of a cold, followed by coughing and sneezing. Most people recover in about 7-10 days. You can help reduce your risk of getting a cold: wash your hands often, avoid close contact with sick people, and don’t touch your face with unwashed hands.
Symptoms
Most people get colds in the winter and spring, but it is possible to get a cold any time of the year. Symptoms usually include:
- sore throat
- runny nose
- coughing
- sneezing
- headaches
- body aches
Most people recover within about 7-10 days. However, people with weakened immune systems, asthma, or respiratory conditions may develop serious illness, such as bronchitis or pneumonia.
Causes of the Common Cold
Many different respiratory viruses can cause the common cold, but rhinoviruses are the most common. Rhinoviruses can also trigger asthma attacks and have been linked to sinus and ear infections. Other viruses that can cause colds include respiratory syncytial virus, human parainfluenza viruses, adenovirus, common human coronaviruses, and human metapneumovirus.
How to Feel Better
There is no cure for a cold. To feel better, you should get lots of rest and drink plenty of fluids. Over-the-counter medicines may help ease symptoms but will not make your cold go away any faster. Always read the label and use medications as directed.
How to Protect Yourself
Viruses that cause colds can spread from infected people to others through the air and close personal contact. You can also get infected through contact with stool (poop) or respiratory secretions from an infected person. This can happen when you shake hands with someone who has a cold, or touch a surface, like a doorknob, that has respiratory viruses on it, then touch your eyes, mouth, or nose.
You can help reduce your risk of getting a cold:
- Wash your hands often with soap and water. Wash them for 20 seconds, and help young children do the same. If soap and water are not available, use an alcohol-based hand sanitizer. Viruses that cause colds can live on your hands, and regular handwashing can help protect you from getting sick.
- Avoid touching your eyes, nose, and mouth with unwashed hands. Viruses that cause colds can enter your body this way and make you sick.
- Stay away from people who are sick. Sick people can spread viruses that cause the common cold through close contact with others.
Source: https://www.cdc.gov/flu/about/keyfacts.htm
COVID-19
What should I do if I feel sick?
Symptoms:
- Cough
- Shortness of breath
- New loss of taste or smell
- Fatigue
- Fever
- Chills
- Headache
- Sore throat
- Muscle or body aches
- Congestion or runny nose
- Diarrhea
- Nausea or vomiting
If you develop these symptoms or have been in close contact with a person known to have COVID-19, call Health Services or your primary healthcare provider.
Faculty and staff should contact Employee Health at 662-915-6550 for additional information.
Students should contact Student Health at 662-915-7274 for additional information.
You can also contact Baptist Memorial Hospital’s 24-hour hotline for additional information – 866-941-4785.
What To Do if You Are Sick — CDC
How do I report my positive COVID-19 result?
There are two ways this can be done.
- Fill out the UHS Self Report form, scan or take a picture of your results and upload both the form and your results to our HIPAA compliant UMBOX. Only University Health Services personnel will be able to view your documentation.
OR
- Students: Call Student Health at 662-915-7274 (Mon, Tues, Wed and Fri, 8 a.m.–5 p.m.; Thurs, 8 a.m.–4 p.m.)
- Employees: Call Employee Health at 662-915-6550 (Mon–Fri, 8 a.m.–5 p.m.)
Where can I get tested for COVID-19 in Oxford?
Both Student and Employee Health have a variety of COVID-19 tests. Call to schedule today!
Besides University Health Services, here are some other clinics in town where you can be tested:
Family Medicine Group of Oxford
1397 Belk Blvd, Oxford, Mississippi
(662) 236-4675
Monday-Thursday 8am-7pm
Friday 8am-5pm
Saturday 9am-3pm, Sunday closed
__________________
Ole Town Med
2580 Jackson Avenue West Suite #44, Oxford, Mississippi
(662) 234-9112
Monday – Friday: 8am – 8pm
Saturday 10am – 4pm
Sunday 12pm – 6pm
__________________
Oxford Family Clinic
1914 University Avenue, Oxford, Mississippi
(662) 238-7860
Monday thru Thursday 8am to 5pm
Friday 8 am to 12 pm
__________________
Oxford Urgent Care
1929 University Ave., Oxford, Misissippi
(662) 236-2232
Open 7 days a week, 8am to 7pm
__________________
RedMed, LLC
1902 B West Jackson Avenue, Oxford, Mississippi
(662) 234-6464
Monday-Friday 7am-7pm
Saturday 9am-5pm
Sunday 1pm-5pm
Walgreens
Sign up here: https://www.walgreens.com/findcare/covid19/testing?ban=covidfy21_newtestingpg_heroban
CVS
Sign up here: https://www.cvs.com/minuteclinic/covid-19-testing
What is the current guidance for isolation and quarantine?
ISOLATION
The updated CDC Respiratory Virus Guidance recommends that people stay home and away from others until at least 24 hours after both their symptoms are getting better overall, and they have not had a fever (and are not using fever-reducing medication). Note that depending on the length of symptoms, this period could be shorter, the same, or longer than the previous guidance for COVID-19.
Source: https://www.cdc.gov/respiratory-viruses/guidance/faq.html
CDC no longer recommends the mandatory 5-day isolation.
QUARANTINE
What is an exposure?
- The current definition of exposure to COVID-19 remains 15 minutes of cumulative contact over a 24-hour period at <6 feet. An infected person can spread COVID-19 up to 2 days before they have symptoms or 2 days prior to positive test if they have no symptoms, therefore, contacts should be identified who were exposed up to 2 days prior to onset or test date accordingly.
Who doesn’t have to quarantine?
- As of August 11, 2022, CDC states that quarantine of exposed persons is no longer recommended regardless of vaccination status.
- CDC states that persons who have had recent confirmed or suspected exposure to an infected person should wear a mask for 10 days around others when indoors in public and should receive testing ≥5 days after exposure (or sooner, if they are symptomatic) regardless of their vaccination status
For more information, please review the updated CDC Guidance on Quarantine and Isolation.
When should I seek medical attention?
If you have any of these emergency warning signs* for COVID-19, get medical attention immediately:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face
*This list is not all inclusive. Please consult your medical provider for any other symptoms that are severe or concerning to you. Call 911 if you have a medical emergency: Notify the operator that you have, or think you might have, COVID-19. If possible, put on a cloth face covering before medical help arrives.
Vaccines & other prevention strategies
Employees and students can walk-in any day to Pharmacy Health Services inside University Health Services for free COVID-19 Vaccines.
The best way to help prevent infection is to avoid being exposed to the virus, and the Centers for Disease Control and Prevention (CDC) recommends a number of preventive actions to follow including:
- GET VACCINATED here:
- Wear a mask indoors or when in tightly packed groups with others.
- Wash your hands often with soap and water for at least 20 seconds. Use an alcohol-based hand sanitizer that contains at least 60% alcohol if soap and water are not available.
- Avoid touching your eyes, nose and mouth with unwashed hands.
- Stay home when you are sick.
- Clean and disinfect frequently touched objects and surfaces.
These are everyday habits that can help prevent the spread of several viruses.
What are current treatment options?
Oral Antivirals
Oral antiviral therapies Paxlovid (Pfizer) and molnupiravir (Merck) are products authorized by the FDA for treatment of COVID-19. These therapies require a prescription from a licensed healthcare provider. Talk to your healthcare provider or pharmacist to see whether an oral antiviral is the right option for you.
How they work: Oral antiviral medications work by targeting specific proteins on the SARS-CoV-2 virus to help prevent the virus replicating within the body. It is important that the oral antiviral is started within 5 days of the start of symptoms.
Who can receive treatment?
People who test positive for COVID-19 with mild to moderate symptoms who are at higher risk for developing more serious COVID-19 symptoms may be eligible for monoclonal antibody or oral antiviral treatment, depending on their health history and exposure to COVID-19, and how long they’ve had symptoms of COVID-19.
What should I do if I think I need them?
If you have tested positive, reach out to Student Health or Employee Health to discuss with a provider.
COVID-19 is stressing me out
It’s normal & understandable to feel anxious, especially if you live in an affected community. If you are feeling increased stress or anxiety, please contact Student Health Services at 662-915-7274 or the University Counseling Center at 662-915-3784. Click here for coping tips.
For more information from the university on COVID-19 response, click here.
FLU
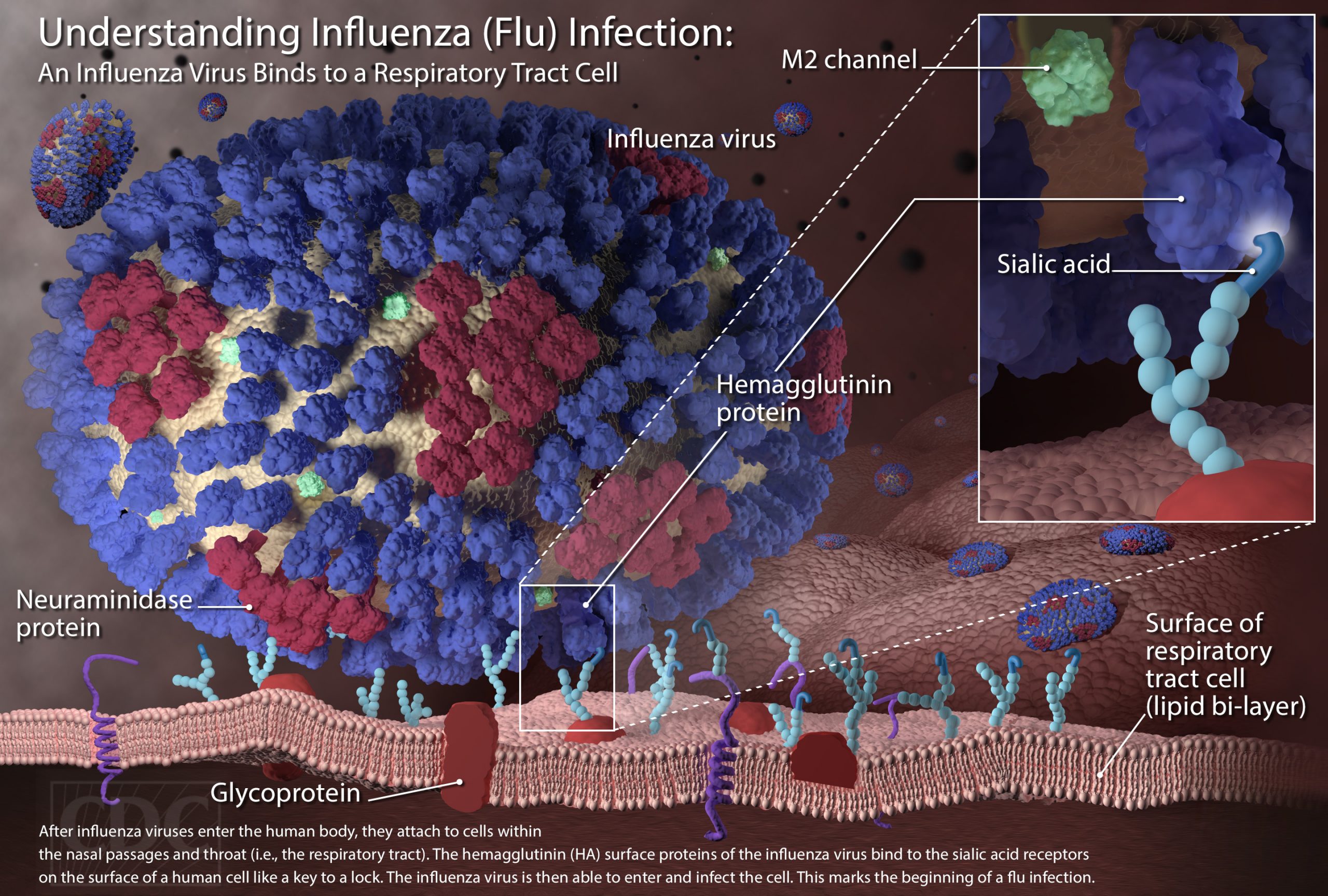
What is Influenza (Flu)?
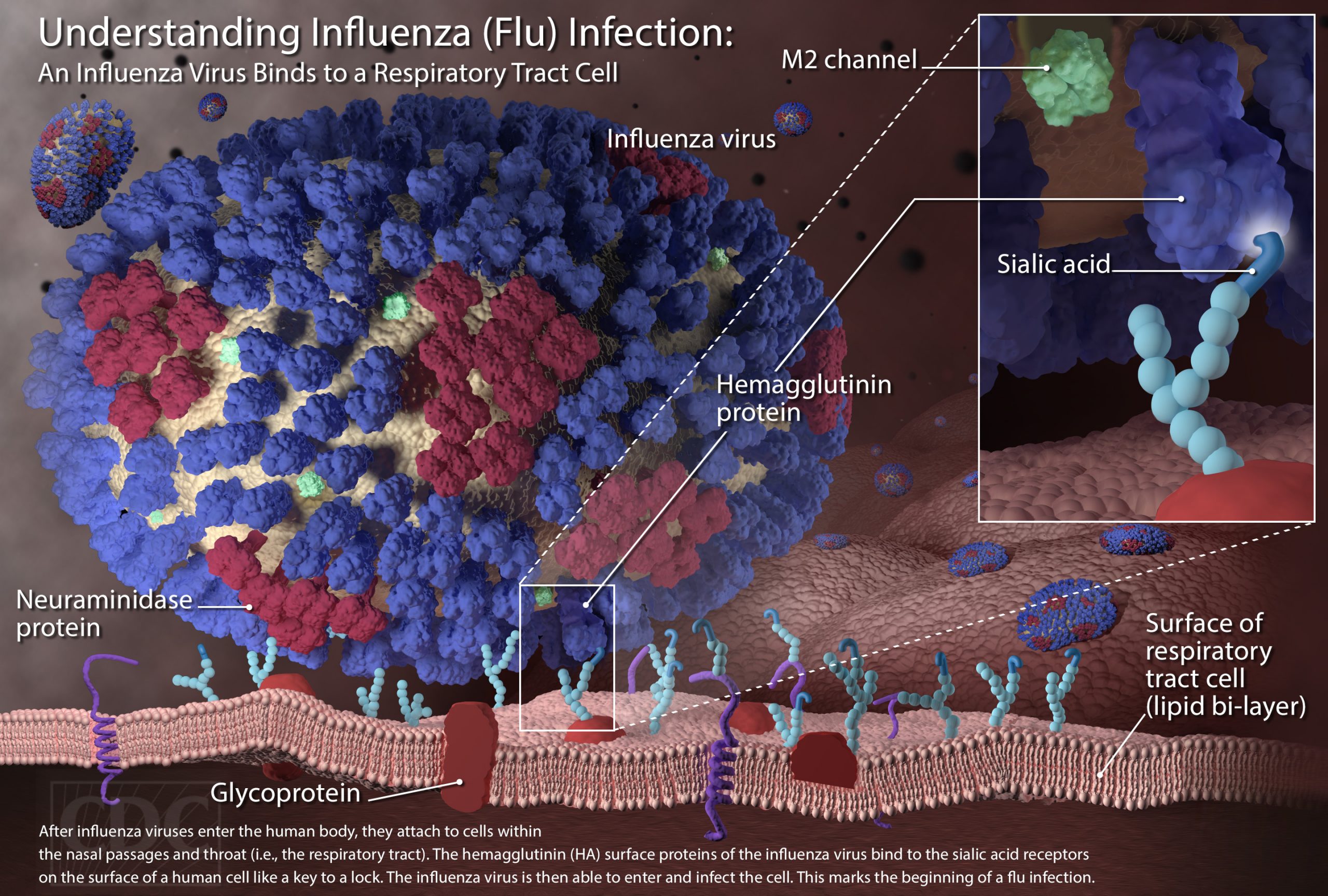
Flu is a contagious respiratory illness caused by influenza viruses that infect the nose, throat, and sometimes the lungs. It can cause mild to severe illness, and at times can lead to death. The best way to prevent flu is by getting a flu vaccine each year.
Flu Symptoms
Influenza (flu) can cause mild to severe illness, and at times can lead to death. Flu symptoms usually come on suddenly. People who have flu often feel some or all of these symptoms:
- fever* or feeling feverish/chills
- cough
- sore throat
- runny or stuffy nose
- muscle or body aches
- headaches
- fatigue (tiredness)
- some people may have vomiting and diarrhea, though this is more common in children than adults.
*It’s important to note that not everyone with flu will have a fever.
More information is available at Flu and COVID-19 symptoms.
How Flu Spreads
Most experts believe that flu viruses spread mainly by tiny droplets made when people with flu cough, sneeze, or talk. These droplets can land in the mouths or noses of people who are nearby. Less often, a person might get flu by touching a surface or object that has flu virus on it and then touching their own mouth, nose or possibly their eyes.
Source: https://www.cdc.gov/flu/about/keyfacts.htm
Message on 2022-2023 Flu Season:
Why do we think flu season will be bad this season?
Countries in the Southern Hemisphere are just finishing up a more severe flu season, which in the past, has forecasted the subsequent season in our Northern Hemisphere. Dr. Spears’s research on the topic has revealed that because of the low rate of flu throughout the world the past two years (due in part to masking and social distancing), we have not had our usual exposure to influenza viruses and our immunity has waned.
How can I protect myself this flu season?
With several companies producing flu vaccines, it can be hard to choose what is best for you. The good news is that no matter which vaccine you choose, you are being protected against the same strains for this season’s virus. Luckily, Dr. Spears states that there are three choices recommended for people aged 65 and over and for the immunocompromised:
- high dose egg-based inactivated (Fluzone),
- the adjuvanted egg-based inactivated (Fluad) and
- the recombinant (Flublok)
There is a nasal spray option (FluMist Quadrivalent) that is a live attenuated vaccine, meaning it contains weakened versions of the flu viruses instead of inactivated viruses. However, it is not safe for asthmatics, children and adolescents taking aspirin, people with cochlear implants, and several other conditions. Due to these complexities, the decision to take the inhaled vaccine should be made with a medical provider.
Where can I get the flu vaccine or treatment?
Pharmacy Health, Student Health, and Employee Health Services can provide the flu vaccine for you on a walk-in basis. The current vaccines we are offering are the Fluarix Quadrivalent and the FluLaval Quadrivalent. If you start experiencing symptoms of flu, call Employee (662.915.6550) or Student Health (662.915.7274) to schedule an appointment for testing and treatment options including antivirals.
How else can I protect myself?
The CDC recommends these tips and more for staying healthy during flu season:
- Cover your mouth and nose when coughing or sneezing
- Practice proper hand hygiene and avoid touching your eyes, nose or mouth
- Stay home when you are sick
The clinicians and staff at University Health Services want you to stay healthy and are here for your healthcare needs.
MELIOIDOSIS

If you caught the headline a while back, it may have been very alarming to see the identification of a bacterium that causes a rare disease called melioidosis. The Centers for Disease Control and Prevention (CDC) identified the Burkholderia pseudomallei (B. pseudomallei) for the first time in the continental United States in our Gulf Coast region of southern Mississippi. As we have with every disease threat, University Health Services wanted to share some information about melioidosis and its impact on our community.
What is melioidosis?
Melioidosis is a rare bacterial infection caused by B. pseudomallei. It is more commonly found in tropical or subtropical areas of the world. It can affect both humans and animals.
How is it spread?
B. pseudomallei usually enters the body when you inhale soil dust or water droplets, touch contaminated soil through cuts in the skin, or by drinking contaminated water.
What are the symptoms?
The symptoms may depend on the location of the infection as discussed above. Those who become infected via skin wounds can experience pain or swelling at the site, fever, ulceration, or abscess. Those who have lung infection can experience cough, chest pain, fever, headache, or decreased appetite. If it enters your blood, symptoms can include fever, weight loss, stomach pain, chest pain, muscle/joint pain, headache, and seizures.
Symptoms can appear 2-4 weeks after exposure, but current data shows it varies.
How is it identified and treated?
Melioidosis is diagnosed through samples from blood, urine, skin lesion, or throat swabs. If it is identified, your provider can treat you with long courses of antibiotics.
How do I prevent exposure?
Avoid exposure to soil or standing water in areas where the disease is common. Always protect open wounds with waterproof dressing. Wear waterproof boots when gardening, doing yard work, or agricultural work – especially after flooding or storms. Wear gloves when working directly with soil. Avoid ingesting unclean water or allowing water to enter your nasal passages when swimming in warm waters.
Most healthy people never develop melioidosis when infected. However, those with chronic illness such as diabetes, kidney disease, or lung disease may be at risk of severe illness from infection.
How does this affect me and the UM community?
It is always important to be aware of new and emerging infectious disease threats. There have only been two identified human cases on the Gulf Coast, and environmental sampling of soil and water during this investigation revealed the bacterium’s presence. At this time, risk for our area is extremely low.
However, it is unclear how long it has been in the environment prior to 2020 or how widespread it is in the continental United States. Modeling suggests that the environmental conditions found in the Gulf Coast states are conducive to the growth of B. pseudomallei. The CDC is currently conducting sampling and case reviews for potentially missed cases over the past few years.
University Health Services collaborates closely with the Mississippi State Department of Health and will continue to monitor this situation and update our campus community as new information is uncovered.
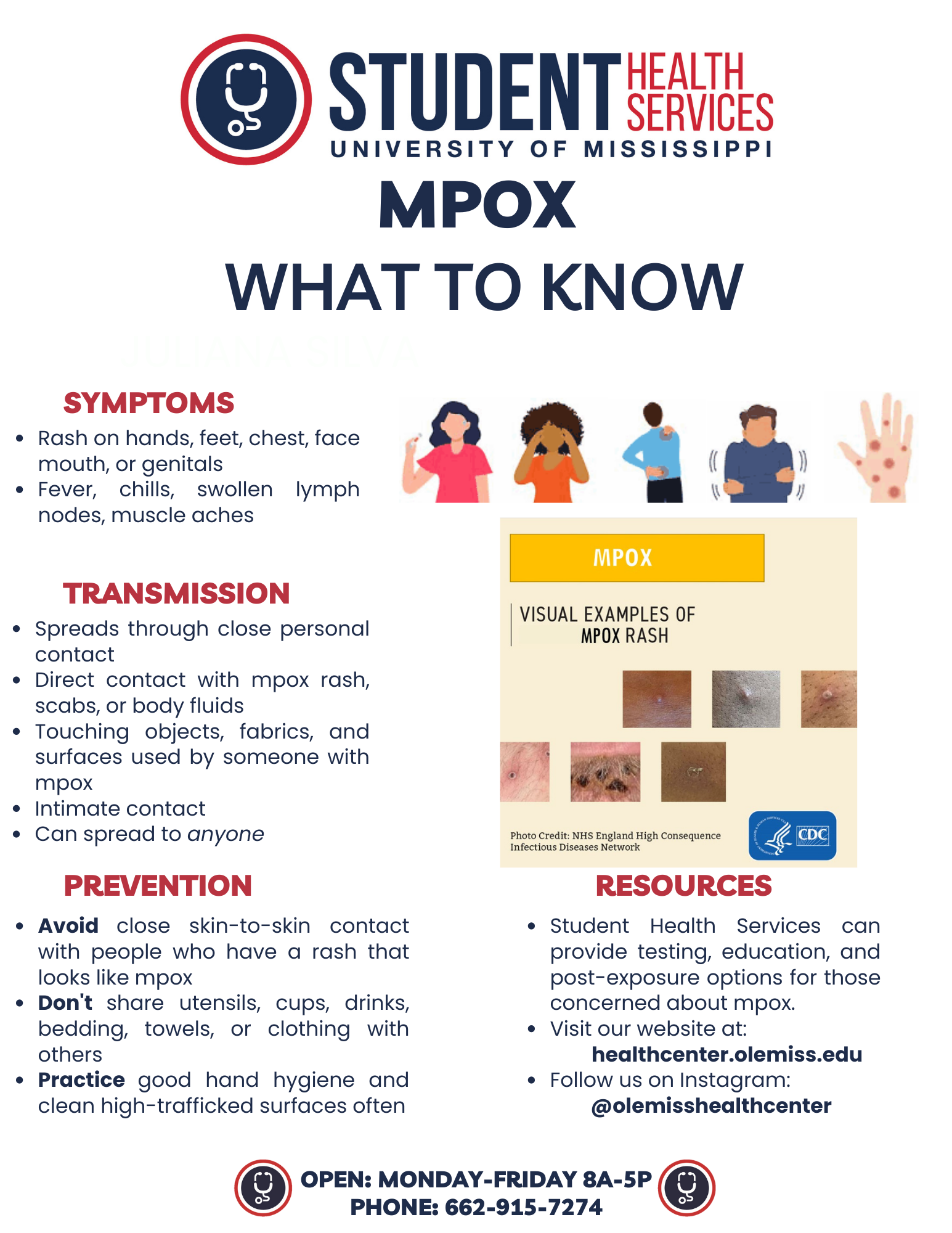
MPOX
*click here for latest UMToday message
*UHS is updating webpages with the term “mpox” to reduce stigma and other issues associated with prior terminology. This change is aligned with the recent World Health Organization
Mpox is a rare disease caused by infection with the mpox virus. Mpox virus is part of the same family of viruses as variola virus, the virus that causes smallpox. Mpox symptoms are similar to smallpox symptoms, but milder, and mpox is rarely fatal. Mpox is not related to chickenpox.
Mpox was discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research. Despite being named “monkeypox,” the source of the disease remains unknown. However, African rodents and non-human primates (like monkeys) might harbor the virus and infect people.
The first human case of mpox was recorded in 1970. Prior to the 2022 outbreak, mpox had been reported in people in several central and western African countries. Previously, almost all mpox cases in people outside of Africa were linked to international travel to countries where the disease commonly occurs or through imported animals. These cases occurred on multiple continents.
Source: https://www.cdc.gov/poxvirus/monkeypox/about.html
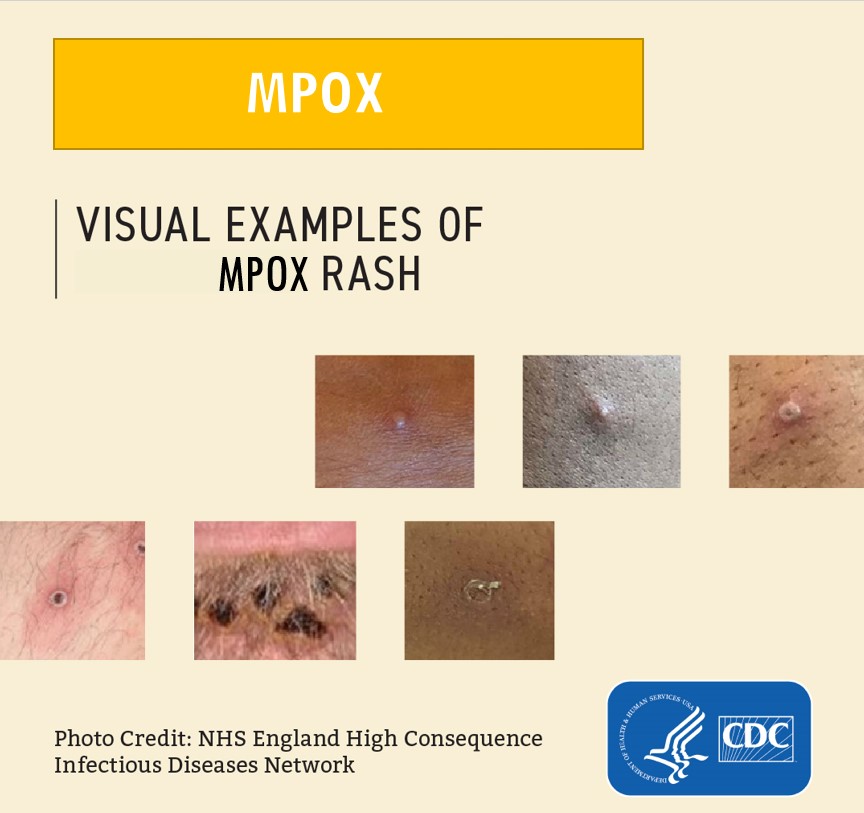
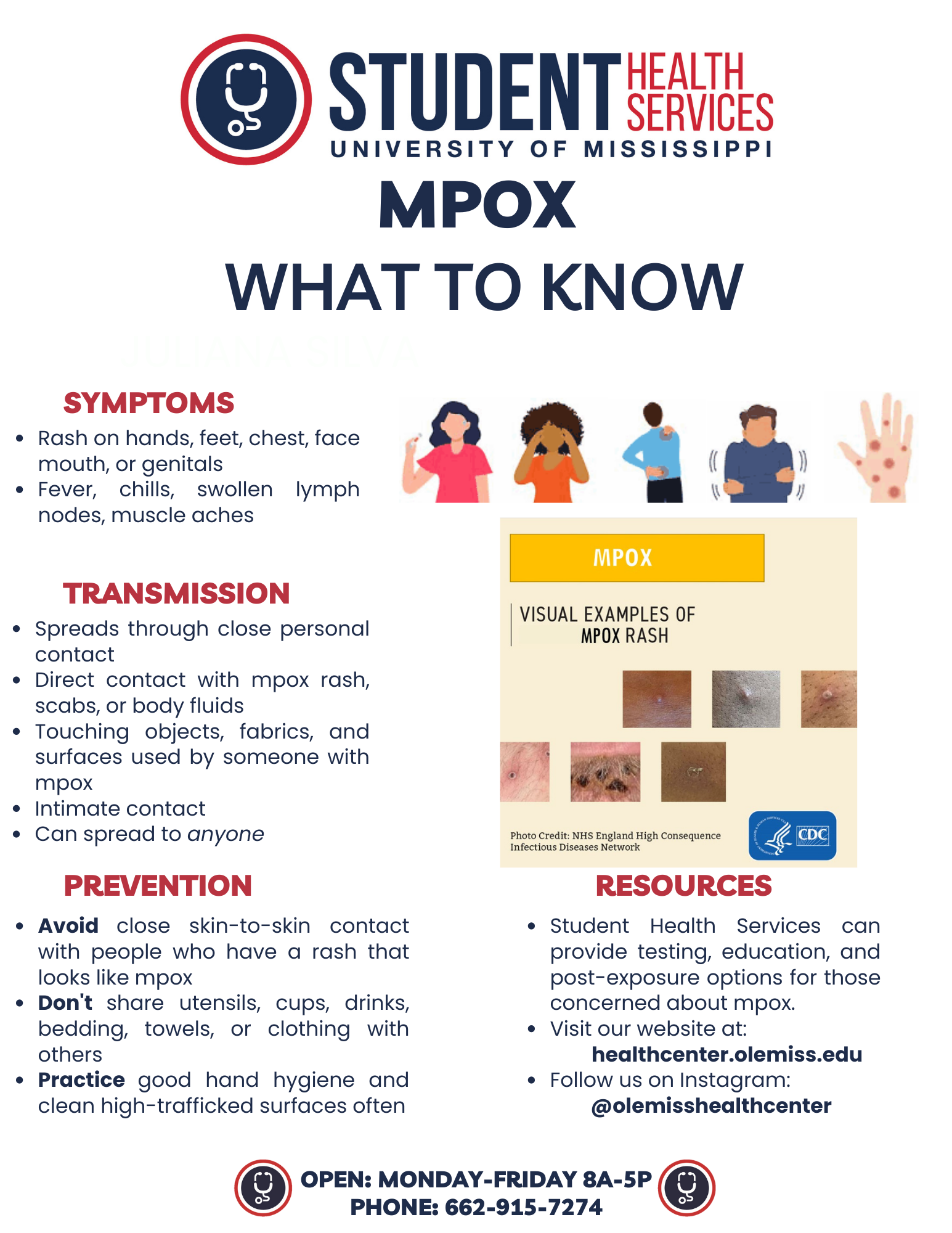
What are the symptoms?
- Fever
- Headache
- Muscle aches and backache
- Swollen lymph nodes
- Chills
- Exhaustion
- Respiratory symptoms (e.g. sore throat, nasal congestion, or cough)
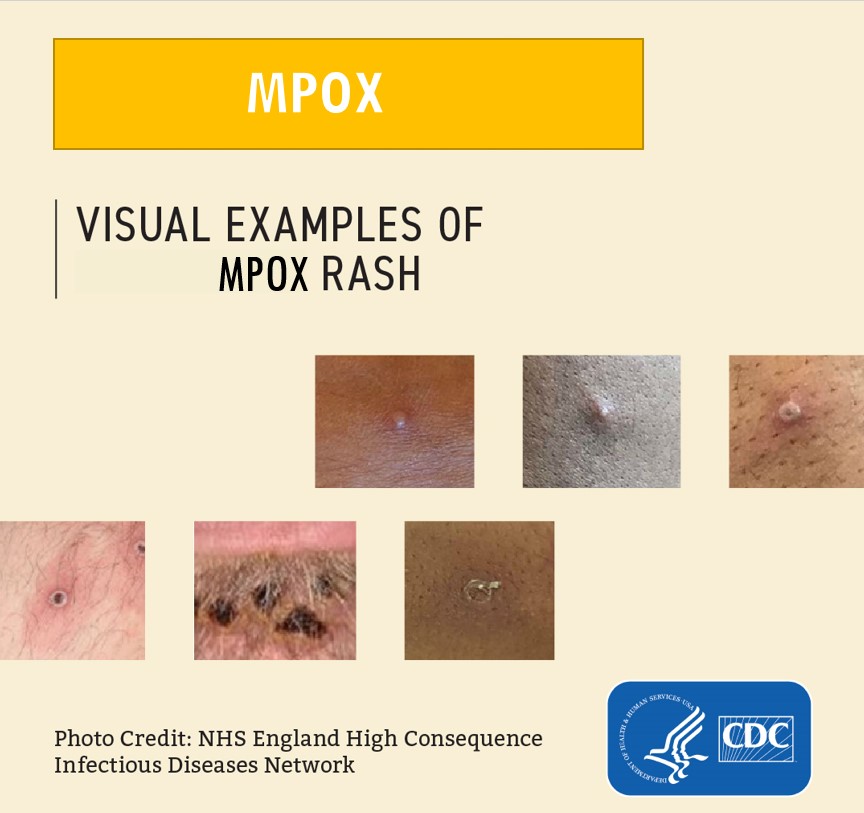
- A rash that may be located on or near the genitals (penis, testicles, labia, and vagina) or anus but could also be on other areas like the hands, feet, chest, face, or mouth.
- The rash will go through several stages, including scabs, before healing.
- The rash can look like pimples or blisters and may be painful or itchy.
You may experience all or only a few symptoms
- Sometimes, people get a rash first, followed by other symptoms. Others only experience a rash.
- Most people with mpox will get a rash.
- Some people have developed a rash before (or without) other symptoms.
Mpox symptoms usually start within 3 weeks of exposure to the virus. If someone has flu-like symptoms, they will usually develop a rash 1-4 days later.
Mpox can be spread from the time symptoms start until the rash has healed, all scabs have fallen off, and a fresh layer of skin has formed. The illness typically lasts 2-4 weeks.
Source: https://www.cdc.gov/poxvirus/monkeypox/symptoms.html
How does it spread?
Mpox spreads in a few ways.
- Mpox can spread to anyone through close, personal, often skin-to-skin contact, including:
- Direct contact with mpox rash, scabs, or body fluids from a person with mpox.
- Touching objects, fabrics (clothing, bedding, or towels), and surfaces that have been used by someone with mpox.
- Contact with respiratory secretions.
- This direct contact can happen during intimate contact, including:
- Oral, anal, and vaginal sex or touching the genitals (penis, testicles, labia, and vagina) or anus of a person with mpox.
- Hugging, massage, and kissing.
- Prolonged face-to-face contact.
- Touching fabrics and objects during sex that were used by a person with mpox and that have not been disinfected, such as bedding, towels, fetish gear, and sex toys.
- A pregnant person can spread the virus to their fetus through the placenta.
It’s also possible for people to get mpox from infected animals, either by being scratched or bitten by the animal or by preparing or eating meat or using products from an infected animal.
A person with mpox can spread it to others from the time symptoms start until the rash has fully healed and a fresh layer of skin has formed. The illness typically lasts 2-4 weeks.
Scientists are still researching:
- If the virus can be spread when someone has no symptoms
- How often mpox is spread through respiratory secretions, or when a person with mpox symptoms might be more likely to spread the virus through respiratory secretions.
- Whether mpox can be spread through semen, vaginal fluids, urine, or feces.
Source: https://www.cdc.gov/poxvirus/monkeypox/transmission.html
How do I protect myself?
Take the following steps to prevent getting mpox:
- Avoid close, skin-to-skin contact with people who have a rash that looks like mpox.
- Do not touch the rash or scabs of a person with mpox.
- Do not kiss, hug, cuddle or have sex with someone with mpox.
- Avoid contact with objects and materials that a person with mpox has used.
- Do not share eating utensils or cups with a person with mpox.
- Do not handle or touch the bedding, towels, or clothing of a person with mpox.
- Wash your hands often with soap and water or use an alcohol-based hand sanitizer, especially before eating or touching your face and after you use the bathroom.
Source: https://www.cdc.gov/poxvirus/monkeypox/prevention/protect-yourself.html
What if I am exposed?
Who should be monitored and for how long?
Anyone with an exposure to people or animals with mpox should monitor their health or be monitored for signs or symptoms consistent with mpox for 21 days after their last exposure.
Do I have to Quarantine?
Individuals exposed to mpox virus can continue their routine daily activities (e.g., go to work or school) as long as they do not have signs or symptoms consistent with mpox. It is important that if you are exposed that you talk to a healthcare provider or answer any communication received from the state health department.
Other Resources
U.S. Map and Case Count
NOROVIRUS
Norovirus is a very contagious virus that causes vomiting and diarrhea. Anyone can get infected and sick with norovirus. You can get norovirus from:
- Having direct contact with an infected person
- Consuming contaminated food or water
- Touching contaminated surfaces and then putting your unwashed hands in your mouth
Norovirus is sometimes called the stomach flu or stomach bug. However, norovirus illness is not related to the flu which is caused by influenza virus.
Symptoms
- Diarrhea
- Vomiting
- Nausea
- Stomach pain
Norovirus causes inflammation of the stomach or intestines. This is called acute gastroenteritis.
A person usually develops symptoms 12 to 48 hours after being exposed to norovirus. Most people with norovirus illness get better within 1 to 3 days.
If you have norovirus illness, you can feel extremely ill, and vomit or have diarrhea many times a day. This can lead to dehydration, especially in young children, older adults, and people with other illnesses.
Prevention
You can help protect yourself and others from norovirus by washing your hands thoroughly with soap and water and following other simple prevention tips.
Practice proper hand hygiene
Wash your hands thoroughly with soap and water
- After using the toilet or changing diapers.
- Before eating, preparing, or handling food.
- Before giving yourself or someone else medicine.
Norovirus can be found in your vomit or feces (poop) even before you start feeling sick. The virus can also stay in your feces for two weeks or more after you feel better. It is important to continue washing your hands often during this time.
Hand sanitizer does not work well against norovirus. Handwashing is always best. Wash your hands with soap and water for at least 20 seconds. You can use hand sanitizers in addition to hand washing, but hand sanitizer is not a substitute for washing your hands with warm water and soap.
Handle and prepare food safely
Before preparing and eating your food:
- Carefully wash fruits and vegetables.
- Cook oysters and other shellfish thoroughly to an internal temperature of at least 145°F .
Be aware that noroviruses are relatively resistant to heat. They can survive temperatures as high as 145°F. Quick steaming processes that are often used for cooking shellfish may not heat foods enough to kill noroviruses.
Food that might be contaminated with norovirus should be thrown out.
People who are sick should not prepare or handle food.
When you are sick, do not prepare food or care for others
You should not prepare food for others or provide healthcare while you are sick and for at least two days after symptoms stop. This also applies to sick workers in restaurants, schools, daycares, long-term care facilities, and other places where they may expose people to norovirus.
Clean and disinfect surfaces
After someone vomits or has diarrhea, always thoroughly clean and disinfect the entire area immediately:
-
Put on rubber or disposable gloves and wipe the entire area with paper towels, then disinfect the area using a bleach-based household cleaner as directed on the product label.
- Leave the bleach disinfectant on the affected area for at least five minutes, then clean the entire area again with soap and hot water. Finish by cleaning soiled laundry, taking out the trash, and washing your hands.
To help make sure that food is safe from norovirus, routinely clean and sanitize kitchen utensils, counters, and surfaces before preparing food.
You should use a chlorine bleach solution with a concentration of 1,000 to 5,000 ppm (5 to 25 tablespoons of household bleach [5% to 8%] per gallon of water) or other disinfectant registered as effective against norovirus by the Environmental Protection Agency (EPA). For more information, see EPA’s Registered Antimicrobial Products Effective Against Norovirus (Norwalk-like virus) [6 pages].
Wash laundry thoroughly
Immediately remove and wash clothes or linens that may be soiled with vomit or feces.
You should:
- Handle soiled items carefully without agitating (shaking) them.
- Wear rubber or disposable gloves while handling soiled items and wash your hands afterwards.
- Wash the items with detergent (cleaning agent) and hot water at the maximum available cycle length and then machine dry them at the highest heat setting.
Treatment
There is no specific medicine to treat people with norovirus illness.
If you have norovirus illness, you should drink plenty of liquids to replace fluid lost from vomiting and diarrhea. This will help prevent dehydration.
Dehydration can lead to serious problems. Severe dehydration may require hospitalization for treatment with fluids given through your vein (intravenous or IV fluids).
Watch for signs of dehydration in children who have norovirus illness. Children who are dehydrated may cry with few or no tears and be unusually sleepy or fussy.
If you think you or someone you are caring for is severely dehydrated, call your healthcare provider.
Antibiotic drugs will not help treat norovirus infections because they fight bacteria, not viruses.
Source: https://www.cdc.gov/norovirus/about/index.html
RSV
Respiratory syncytial virus, or RSV, is a common respiratory virus that usually causes mild, cold-like symptoms. Most people recover in a week or two, but RSV can be serious, especially for infants and older adults. RSV is the most common cause of bronchiolitis (inflammation of the small airways in the lung) and pneumonia (infection of the lungs) in children younger than 1 year of age in the United States.
Symptoms
People infected with RSV usually show symptoms within 4 to 6 days after getting infected. Symptoms of RSV infection usually include
- Runny nose
- Decrease in appetite
- Coughing
- Sneezing
- Fever
- Wheezing
These symptoms usually appear in stages and not all at once. In very young infants with RSV, the only symptoms may be irritability, decreased activity, and breathing difficulties. Almost all children will have had an RSV infection by their second birthday.
How it’s spread
RSV can spread when
- An infected person coughs or sneezes
- You get virus droplets from a cough or sneeze in your eyes, nose, or mouth
- You have direct contact with the virus, like kissing the face of a child with RSV
- You touch a surface that has the virus on it, like a doorknob, and then touch your face before washing your hands
People infected with RSV are usually contagious for 3 to 8 days and may become contagious a day or two before they start showing signs of illness. However, some infants, and people with weakened immune systems, can continue to spread the virus even after they stop showing symptoms, for as long as 4 weeks. Children are often exposed to and infected with RSV outside the home, such as in school or childcare centers. They can then transmit the virus to other members of the family.
RSV can survive for many hours on hard surfaces such as tables and crib rails. It typically lives on soft surfaces such as tissues and hands for shorter amounts of time.
People are typically infected with RSV for the first time as an infant or toddler and nearly all children are infected before their second birthday. However, repeat infections may occur throughout life, and people of any age can be infected. Infections in healthy children and adults are generally less severe than among infants and older adults with certain medical conditions. People at highest risk for severe disease include
- Premature infants
- Young children with congenital (from birth) heart or chronic lung disease
- Young children with compromised (weakened) immune systems due to a medical condition or medical treatment
- Children with neuromuscular disorders
- Adults with compromised immune systems
- Older adults, especially those with underlying heart or lung disease
In the United States and other areas with similar climates, RSV circulation generally starts during fall and peaks in the winter. The timing and severity of RSV circulation in a given community can vary from year to year.
Care
Most RSV infections go away on their own in a week or two.
There is no specific treatment for RSV infection, though researchers are working to develop vaccines and antivirals (medicines that fight viruses).
Steps to relieve symptoms:
- Manage fever and pain with over-the-counter fever reducers and pain relievers, such as acetaminophen or ibuprofen. (Never give aspirin to children.)
- Drink enough fluids. It is important for people with RSV infection to drink enough fluids to prevent dehydration (loss of body fluids).
- Talk to your healthcare provider before giving your child nonprescription cold medicines. Some medicines contain ingredients that are not good for children.
Prevention
There are steps you can take to help prevent the spread of RSV. Specifically, if you have cold-like symptoms you should
- Cover your coughs and sneezes with a tissue or your upper shirt sleeve, not your hands
- Wash your hands often with soap and water for at least 20 seconds
- Avoid close contact, such as kissing, shaking hands, and sharing cups and eating utensils, with others
- Clean frequently touched surfaces such as doorknobs and mobile devices
Ideally, people with cold-like symptoms should not interact with children at high risk for severe RSV disease, including premature infants, children younger than 2 years of age with chronic lung or heart conditions, children with weakened immune systems, or children with neuromuscular disorders. If this is not possible, they should carefully follow the prevention steps mentioned above and wash their hands before interacting with such children. They should also refrain from kissing high-risk children while they have cold-like symptoms.
Parents of children at high risk for developing severe RSV disease should help their child, when possible, do the following
- Avoid close contact with sick people
- Wash their hands often with soap and water for at least 20 seconds
- Avoid touching their face with unwashed hands
- Limit the time they spend in childcare centers or other potentially contagious settings during periods of high RSV activity. This may help prevent infection and spread of the virus during the RSV season
Source: https://www.cdc.gov/flu/about/keyfacts.htm
ZIKA
What is it?
-
- Zika virus was first discovered in 1947 and is named after the Zika Forest in Uganda. In 1952, the first human cases of Zika were detected and since then, outbreaks of Zika have been reported in tropical Africa, Southeast Asia, and the Pacific Islands.
- Zika is spread mostly by the bite of an infected Aedes species mosquito (Ae. aegypti and Ae. albopictus). These mosquitoes bite during the day and night.
Why is it a concern?
-
- Zika can be passed from a pregnant woman to her fetus. Infection during pregnancy can cause certain birth defects.
- There is no vaccine or medicine for Zika.
How is it spread?
- Through mosquito bites
- From a pregnant woman to her fetus
- Through sex
How do I prevent it?
Clothing
- Wear long-sleeved shirts and long pants.
- Treat your clothing and gear with permethrin or buy pre-treated items.
Insect repellent
- Use Environmental Protection Agency (EPA)-registered insect repellents with one of the following active ingredients:
DEET, picaridin, IR3535, oil of lemon eucalyptus or para-menthane-diol, or 2-undecanone. Always follow the product label instructions.
- When used as directed, these insect repellents are proven safe and effective even for pregnant and breastfeeding women.
- Do not use products containing oil of lemon eucalyptus or para-menthane-diol on children younger than 3 years old.
At Home
- Stay in places with air conditioning and window and door screens to keep mosquitoes outside.
- Take steps to control mosquitoes inside and outside your home.
- Mosquito netting can be used to cover babies younger than 2 months old in carriers, strollers, or cribs.
- Sleep under a mosquito bed net if air conditioned or screened rooms are not available or if sleeping outdoors.
Sexual transmission
- Prevent sexual transmission of Zika by using condoms or not having sex.
What to do if you have Zika:
There is no specific medicine or vaccine for Zika virus. Treat the symptoms:
- Get plenty of rest.
- Drink fluids to prevent dehydration.
- Take medicine such as acetaminophen to reduce fever and pain.
- Do not take aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs).
- If you are taking medicine for another medical condition, talk to your healthcare provider before taking additional medication.
What is Influenza (Flu)?
Flu is a contagious respiratory illness caused by influenza viruses that infect the nose, throat, and sometimes the lungs. It can cause mild to severe illness, and at times can lead to death. The best way to prevent flu is by getting a flu vaccine each year.
Flu Symptoms
Influenza (flu) can cause mild to severe illness, and at times can lead to death. Flu symptoms usually come on suddenly. People who have flu often feel some or all of these symptoms:
- fever* or feeling feverish/chills
- cough
- sore throat
- runny or stuffy nose
- muscle or body aches
- headaches
- fatigue (tiredness)
- some people may have vomiting and diarrhea, though this is more common in children than adults.
*It’s important to note that not everyone with flu will have a fever.
More information is available at Flu and COVID-19 symptoms.
How Flu Spreads
Most experts believe that flu viruses spread mainly by tiny droplets made when people with flu cough, sneeze, or talk. These droplets can land in the mouths or noses of people who are nearby. Less often, a person might get flu by touching a surface or object that has flu virus on it and then touching their own mouth, nose or possibly their eyes.
Source: https://www.cdc.gov/flu/about/keyfacts.htm
Message on 2022-2023 Flu Season:
Why do we think flu season will be bad this season?
Countries in the Southern Hemisphere are just finishing up a more severe flu season, which in the past, has forecasted the subsequent season in our Northern Hemisphere. Dr. Spears’s research on the topic has revealed that because of the low rate of flu throughout the world the past two years (due in part to masking and social distancing), we have not had our usual exposure to influenza viruses and our immunity has waned.
How can I protect myself this flu season?
With several companies producing flu vaccines, it can be hard to choose what is best for you. The good news is that no matter which vaccine you choose, you are being protected against the same strains for this season’s virus. Luckily, Dr. Spears states that there are three choices recommended for people aged 65 and over and for the immunocompromised:
- high dose egg-based inactivated (Fluzone),
- the adjuvanted egg-based inactivated (Fluad) and
- the recombinant (Flublok)
There is a nasal spray option (FluMist Quadrivalent) that is a live attenuated vaccine, meaning it contains weakened versions of the flu viruses instead of inactivated viruses. However, it is not safe for asthmatics, children and adolescents taking aspirin, people with cochlear implants, and several other conditions. Due to these complexities, the decision to take the inhaled vaccine should be made with a medical provider.
Where can I get the flu vaccine or treatment?
Pharmacy Health, Student Health, and Employee Health Services can provide the flu vaccine for you on a walk-in basis. The current vaccines we are offering are the Fluarix Quadrivalent and the FluLaval Quadrivalent. If you start experiencing symptoms of flu, call Employee (662.915.6550) or Student Health (662.915.7274) to schedule an appointment for testing and treatment options including antivirals.
How else can I protect myself?
The CDC recommends these tips and more for staying healthy during flu season:
- Cover your mouth and nose when coughing or sneezing
- Practice proper hand hygiene and avoid touching your eyes, nose or mouth
- Stay home when you are sick
The clinicians and staff at University Health Services want you to stay healthy and are here for your healthcare needs.
MELIOIDOSIS

If you caught the headline a while back, it may have been very alarming to see the identification of a bacterium that causes a rare disease called melioidosis. The Centers for Disease Control and Prevention (CDC) identified the Burkholderia pseudomallei (B. pseudomallei) for the first time in the continental United States in our Gulf Coast region of southern Mississippi. As we have with every disease threat, University Health Services wanted to share some information about melioidosis and its impact on our community.
What is melioidosis?
Melioidosis is a rare bacterial infection caused by B. pseudomallei. It is more commonly found in tropical or subtropical areas of the world. It can affect both humans and animals.
How is it spread?
B. pseudomallei usually enters the body when you inhale soil dust or water droplets, touch contaminated soil through cuts in the skin, or by drinking contaminated water.
What are the symptoms?
The symptoms may depend on the location of the infection as discussed above. Those who become infected via skin wounds can experience pain or swelling at the site, fever, ulceration, or abscess. Those who have lung infection can experience cough, chest pain, fever, headache, or decreased appetite. If it enters your blood, symptoms can include fever, weight loss, stomach pain, chest pain, muscle/joint pain, headache, and seizures.
Symptoms can appear 2-4 weeks after exposure, but current data shows it varies.
How is it identified and treated?
Melioidosis is diagnosed through samples from blood, urine, skin lesion, or throat swabs. If it is identified, your provider can treat you with long courses of antibiotics.
How do I prevent exposure?
Avoid exposure to soil or standing water in areas where the disease is common. Always protect open wounds with waterproof dressing. Wear waterproof boots when gardening, doing yard work, or agricultural work – especially after flooding or storms. Wear gloves when working directly with soil. Avoid ingesting unclean water or allowing water to enter your nasal passages when swimming in warm waters.
Most healthy people never develop melioidosis when infected. However, those with chronic illness such as diabetes, kidney disease, or lung disease may be at risk of severe illness from infection.
How does this affect me and the UM community?
It is always important to be aware of new and emerging infectious disease threats. There have only been two identified human cases on the Gulf Coast, and environmental sampling of soil and water during this investigation revealed the bacterium’s presence. At this time, risk for our area is extremely low.
However, it is unclear how long it has been in the environment prior to 2020 or how widespread it is in the continental United States. Modeling suggests that the environmental conditions found in the Gulf Coast states are conducive to the growth of B. pseudomallei. The CDC is currently conducting sampling and case reviews for potentially missed cases over the past few years.
University Health Services collaborates closely with the Mississippi State Department of Health and will continue to monitor this situation and update our campus community as new information is uncovered.
MPOX
*click here for latest UMToday message
*UHS is updating webpages with the term “mpox” to reduce stigma and other issues associated with prior terminology. This change is aligned with the recent World Health Organization
Mpox is a rare disease caused by infection with the mpox virus. Mpox virus is part of the same family of viruses as variola virus, the virus that causes smallpox. Mpox symptoms are similar to smallpox symptoms, but milder, and mpox is rarely fatal. Mpox is not related to chickenpox.
Mpox was discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research. Despite being named “monkeypox,” the source of the disease remains unknown. However, African rodents and non-human primates (like monkeys) might harbor the virus and infect people.
The first human case of mpox was recorded in 1970. Prior to the 2022 outbreak, mpox had been reported in people in several central and western African countries. Previously, almost all mpox cases in people outside of Africa were linked to international travel to countries where the disease commonly occurs or through imported animals. These cases occurred on multiple continents.
Source: https://www.cdc.gov/poxvirus/monkeypox/about.html
What are the symptoms?
- Fever
- Headache
- Muscle aches and backache
- Swollen lymph nodes
- Chills
- Exhaustion
- Respiratory symptoms (e.g. sore throat, nasal congestion, or cough)
- A rash that may be located on or near the genitals (penis, testicles, labia, and vagina) or anus but could also be on other areas like the hands, feet, chest, face, or mouth.
- The rash will go through several stages, including scabs, before healing.
- The rash can look like pimples or blisters and may be painful or itchy.
You may experience all or only a few symptoms
- Sometimes, people get a rash first, followed by other symptoms. Others only experience a rash.
- Most people with mpox will get a rash.
- Some people have developed a rash before (or without) other symptoms.
Mpox symptoms usually start within 3 weeks of exposure to the virus. If someone has flu-like symptoms, they will usually develop a rash 1-4 days later.
Mpox can be spread from the time symptoms start until the rash has healed, all scabs have fallen off, and a fresh layer of skin has formed. The illness typically lasts 2-4 weeks.
Source: https://www.cdc.gov/poxvirus/monkeypox/symptoms.html
How does it spread?
Mpox spreads in a few ways.
- Mpox can spread to anyone through close, personal, often skin-to-skin contact, including:
- Direct contact with mpox rash, scabs, or body fluids from a person with mpox.
- Touching objects, fabrics (clothing, bedding, or towels), and surfaces that have been used by someone with mpox.
- Contact with respiratory secretions.
- This direct contact can happen during intimate contact, including:
- Oral, anal, and vaginal sex or touching the genitals (penis, testicles, labia, and vagina) or anus of a person with mpox.
- Hugging, massage, and kissing.
- Prolonged face-to-face contact.
- Touching fabrics and objects during sex that were used by a person with mpox and that have not been disinfected, such as bedding, towels, fetish gear, and sex toys.
- A pregnant person can spread the virus to their fetus through the placenta.
It’s also possible for people to get mpox from infected animals, either by being scratched or bitten by the animal or by preparing or eating meat or using products from an infected animal.
A person with mpox can spread it to others from the time symptoms start until the rash has fully healed and a fresh layer of skin has formed. The illness typically lasts 2-4 weeks.
Scientists are still researching:
- If the virus can be spread when someone has no symptoms
- How often mpox is spread through respiratory secretions, or when a person with mpox symptoms might be more likely to spread the virus through respiratory secretions.
- Whether mpox can be spread through semen, vaginal fluids, urine, or feces.
Source: https://www.cdc.gov/poxvirus/monkeypox/transmission.html
How do I protect myself?
Take the following steps to prevent getting mpox:
- Avoid close, skin-to-skin contact with people who have a rash that looks like mpox.
- Do not touch the rash or scabs of a person with mpox.
- Do not kiss, hug, cuddle or have sex with someone with mpox.
- Avoid contact with objects and materials that a person with mpox has used.
- Do not share eating utensils or cups with a person with mpox.
- Do not handle or touch the bedding, towels, or clothing of a person with mpox.
- Wash your hands often with soap and water or use an alcohol-based hand sanitizer, especially before eating or touching your face and after you use the bathroom.
Source: https://www.cdc.gov/poxvirus/monkeypox/prevention/protect-yourself.html
What if I am exposed?
Who should be monitored and for how long?
Anyone with an exposure to people or animals with mpox should monitor their health or be monitored for signs or symptoms consistent with mpox for 21 days after their last exposure.
Do I have to Quarantine?
Individuals exposed to mpox virus can continue their routine daily activities (e.g., go to work or school) as long as they do not have signs or symptoms consistent with mpox. It is important that if you are exposed that you talk to a healthcare provider or answer any communication received from the state health department.
Other Resources
U.S. Map and Case Count
NOROVIRUS
Norovirus is a very contagious virus that causes vomiting and diarrhea. Anyone can get infected and sick with norovirus. You can get norovirus from:
- Having direct contact with an infected person
- Consuming contaminated food or water
- Touching contaminated surfaces and then putting your unwashed hands in your mouth
Norovirus is sometimes called the stomach flu or stomach bug. However, norovirus illness is not related to the flu which is caused by influenza virus.
Symptoms
- Diarrhea
- Vomiting
- Nausea
- Stomach pain
Norovirus causes inflammation of the stomach or intestines. This is called acute gastroenteritis.
A person usually develops symptoms 12 to 48 hours after being exposed to norovirus. Most people with norovirus illness get better within 1 to 3 days.
If you have norovirus illness, you can feel extremely ill, and vomit or have diarrhea many times a day. This can lead to dehydration, especially in young children, older adults, and people with other illnesses.
Prevention
You can help protect yourself and others from norovirus by washing your hands thoroughly with soap and water and following other simple prevention tips.
Practice proper hand hygiene
Wash your hands thoroughly with soap and water
- After using the toilet or changing diapers.
- Before eating, preparing, or handling food.
- Before giving yourself or someone else medicine.
Norovirus can be found in your vomit or feces (poop) even before you start feeling sick. The virus can also stay in your feces for two weeks or more after you feel better. It is important to continue washing your hands often during this time.
Hand sanitizer does not work well against norovirus. Handwashing is always best. Wash your hands with soap and water for at least 20 seconds. You can use hand sanitizers in addition to hand washing, but hand sanitizer is not a substitute for washing your hands with warm water and soap.
Before preparing and eating your food:
- Carefully wash fruits and vegetables.
- Cook oysters and other shellfish thoroughly to an internal temperature of at least 145°F .
Be aware that noroviruses are relatively resistant to heat. They can survive temperatures as high as 145°F. Quick steaming processes that are often used for cooking shellfish may not heat foods enough to kill noroviruses.
Food that might be contaminated with norovirus should be thrown out.
People who are sick should not prepare or handle food.
When you are sick, do not prepare food or care for others
You should not prepare food for others or provide healthcare while you are sick and for at least two days after symptoms stop. This also applies to sick workers in restaurants, schools, daycares, long-term care facilities, and other places where they may expose people to norovirus.
Clean and disinfect surfaces
After someone vomits or has diarrhea, always thoroughly clean and disinfect the entire area immediately:
-
Put on rubber or disposable gloves and wipe the entire area with paper towels, then disinfect the area using a bleach-based household cleaner as directed on the product label.
- Leave the bleach disinfectant on the affected area for at least five minutes, then clean the entire area again with soap and hot water. Finish by cleaning soiled laundry, taking out the trash, and washing your hands.
To help make sure that food is safe from norovirus, routinely clean and sanitize kitchen utensils, counters, and surfaces before preparing food.
You should use a chlorine bleach solution with a concentration of 1,000 to 5,000 ppm (5 to 25 tablespoons of household bleach [5% to 8%] per gallon of water) or other disinfectant registered as effective against norovirus by the Environmental Protection Agency (EPA). For more information, see EPA’s Registered Antimicrobial Products Effective Against Norovirus (Norwalk-like virus) [6 pages].
Wash laundry thoroughly
Immediately remove and wash clothes or linens that may be soiled with vomit or feces.
You should:
- Handle soiled items carefully without agitating (shaking) them.
- Wear rubber or disposable gloves while handling soiled items and wash your hands afterwards.
- Wash the items with detergent (cleaning agent) and hot water at the maximum available cycle length and then machine dry them at the highest heat setting.
Treatment
There is no specific medicine to treat people with norovirus illness.
If you have norovirus illness, you should drink plenty of liquids to replace fluid lost from vomiting and diarrhea. This will help prevent dehydration.
Dehydration can lead to serious problems. Severe dehydration may require hospitalization for treatment with fluids given through your vein (intravenous or IV fluids).
Watch for signs of dehydration in children who have norovirus illness. Children who are dehydrated may cry with few or no tears and be unusually sleepy or fussy.
If you think you or someone you are caring for is severely dehydrated, call your healthcare provider.
Antibiotic drugs will not help treat norovirus infections because they fight bacteria, not viruses.
Source: https://www.cdc.gov/norovirus/about/index.html
RSV
Respiratory syncytial virus, or RSV, is a common respiratory virus that usually causes mild, cold-like symptoms. Most people recover in a week or two, but RSV can be serious, especially for infants and older adults. RSV is the most common cause of bronchiolitis (inflammation of the small airways in the lung) and pneumonia (infection of the lungs) in children younger than 1 year of age in the United States.
Symptoms
People infected with RSV usually show symptoms within 4 to 6 days after getting infected. Symptoms of RSV infection usually include
- Runny nose
- Decrease in appetite
- Coughing
- Sneezing
- Fever
- Wheezing
These symptoms usually appear in stages and not all at once. In very young infants with RSV, the only symptoms may be irritability, decreased activity, and breathing difficulties. Almost all children will have had an RSV infection by their second birthday.
How it’s spread
RSV can spread when
- An infected person coughs or sneezes
- You get virus droplets from a cough or sneeze in your eyes, nose, or mouth
- You have direct contact with the virus, like kissing the face of a child with RSV
- You touch a surface that has the virus on it, like a doorknob, and then touch your face before washing your hands
People infected with RSV are usually contagious for 3 to 8 days and may become contagious a day or two before they start showing signs of illness. However, some infants, and people with weakened immune systems, can continue to spread the virus even after they stop showing symptoms, for as long as 4 weeks. Children are often exposed to and infected with RSV outside the home, such as in school or childcare centers. They can then transmit the virus to other members of the family.
RSV can survive for many hours on hard surfaces such as tables and crib rails. It typically lives on soft surfaces such as tissues and hands for shorter amounts of time.
People are typically infected with RSV for the first time as an infant or toddler and nearly all children are infected before their second birthday. However, repeat infections may occur throughout life, and people of any age can be infected. Infections in healthy children and adults are generally less severe than among infants and older adults with certain medical conditions. People at highest risk for severe disease include
- Premature infants
- Young children with congenital (from birth) heart or chronic lung disease
- Young children with compromised (weakened) immune systems due to a medical condition or medical treatment
- Children with neuromuscular disorders
- Adults with compromised immune systems
- Older adults, especially those with underlying heart or lung disease
In the United States and other areas with similar climates, RSV circulation generally starts during fall and peaks in the winter. The timing and severity of RSV circulation in a given community can vary from year to year.
Care
Most RSV infections go away on their own in a week or two.
There is no specific treatment for RSV infection, though researchers are working to develop vaccines and antivirals (medicines that fight viruses).
Steps to relieve symptoms:
- Manage fever and pain with over-the-counter fever reducers and pain relievers, such as acetaminophen or ibuprofen. (Never give aspirin to children.)
- Drink enough fluids. It is important for people with RSV infection to drink enough fluids to prevent dehydration (loss of body fluids).
- Talk to your healthcare provider before giving your child nonprescription cold medicines. Some medicines contain ingredients that are not good for children.
Prevention
There are steps you can take to help prevent the spread of RSV. Specifically, if you have cold-like symptoms you should
- Cover your coughs and sneezes with a tissue or your upper shirt sleeve, not your hands
- Wash your hands often with soap and water for at least 20 seconds
- Avoid close contact, such as kissing, shaking hands, and sharing cups and eating utensils, with others
- Clean frequently touched surfaces such as doorknobs and mobile devices
Ideally, people with cold-like symptoms should not interact with children at high risk for severe RSV disease, including premature infants, children younger than 2 years of age with chronic lung or heart conditions, children with weakened immune systems, or children with neuromuscular disorders. If this is not possible, they should carefully follow the prevention steps mentioned above and wash their hands before interacting with such children. They should also refrain from kissing high-risk children while they have cold-like symptoms.
Parents of children at high risk for developing severe RSV disease should help their child, when possible, do the following
- Avoid close contact with sick people
- Wash their hands often with soap and water for at least 20 seconds
- Avoid touching their face with unwashed hands
- Limit the time they spend in childcare centers or other potentially contagious settings during periods of high RSV activity. This may help prevent infection and spread of the virus during the RSV season
Source: https://www.cdc.gov/flu/about/keyfacts.htm
ZIKA
What is it?
-
- Zika virus was first discovered in 1947 and is named after the Zika Forest in Uganda. In 1952, the first human cases of Zika were detected and since then, outbreaks of Zika have been reported in tropical Africa, Southeast Asia, and the Pacific Islands.
- Zika is spread mostly by the bite of an infected Aedes species mosquito (Ae. aegypti and Ae. albopictus). These mosquitoes bite during the day and night.
Why is it a concern?
-
- Zika can be passed from a pregnant woman to her fetus. Infection during pregnancy can cause certain birth defects.
- There is no vaccine or medicine for Zika.
How is it spread?
- Through mosquito bites
- From a pregnant woman to her fetus
- Through sex
How do I prevent it?
Clothing
- Wear long-sleeved shirts and long pants.
- Treat your clothing and gear with permethrin or buy pre-treated items.
Insect repellent
- Use Environmental Protection Agency (EPA)-registered insect repellents with one of the following active ingredients:
DEET, picaridin, IR3535, oil of lemon eucalyptus or para-menthane-diol, or 2-undecanone. Always follow the product label instructions. - When used as directed, these insect repellents are proven safe and effective even for pregnant and breastfeeding women.
- Do not use products containing oil of lemon eucalyptus or para-menthane-diol on children younger than 3 years old.
At Home
- Stay in places with air conditioning and window and door screens to keep mosquitoes outside.
- Take steps to control mosquitoes inside and outside your home.
- Mosquito netting can be used to cover babies younger than 2 months old in carriers, strollers, or cribs.
- Sleep under a mosquito bed net if air conditioned or screened rooms are not available or if sleeping outdoors.
Sexual transmission
- Prevent sexual transmission of Zika by using condoms or not having sex.
What to do if you have Zika:
There is no specific medicine or vaccine for Zika virus. Treat the symptoms:
- Get plenty of rest.
- Drink fluids to prevent dehydration.
- Take medicine such as acetaminophen to reduce fever and pain.
- Do not take aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs).
- If you are taking medicine for another medical condition, talk to your healthcare provider before taking additional medication.


